Diagnosis: Pigmented Bowen’s disease
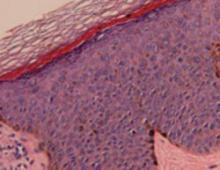
Histopathological evaluation of the lesion revealed hyperkeratosis, large atypical keratinocytes, increased mitotic figures, and an intact basement membrane (FIGURE 2), leading us to diagnose pigmented Bowen’s disease.
Bowen’s disease, an intraepidermal squamous cell carcinoma (carcinoma in situ), is a common type of nonmelanoma skin cancer. However, the form our patient had—pigmented Bowen’s disease—is a rare form of squamous cell carcinoma (SCC) in situ (2% of cases).1 The pigmented form of Bowen’s disease is more common in individuals with darker skin tones, while the nonpigmented is more common in fair-skinned individuals.
Bowen’s disease typically presents as a slow-growing, sharply demarcated, scaly erythematous plaque ranging in size from a few millimeters to several centimeters. Crusting, fissuring, hyperkeratosis, and pigmentation, as seen in our case, are also associated findings.2 Bowen’s disease often presents as a solitary lesion, with most cases (approximately 75%) associated with sun damage.3
The most common sites for Bowen’s disease include the head, neck, and hands. Rarely, the nail bed, oral mucosa, or anogenital region may be affected.
The mean age of diagnosis occurs in the sixth decade4 and there is an equal incidence in men and women. Bowen’s disease in men usually occurs on the scalp and ears, while in women, the lower legs are the most common site.5 Three to eight percent of Bowen’s disease cases progress to invasive carcinoma if left untreated.6
FIGURE 2
Histopathology of pigmented Bowen’s disease