A 57-year-old woman with a history of breast cancer comes to your office complaining of pain and swelling on the left side of her neck. She has recently had a mastectomy and chemotherapy; her port was removed in the past week. She has no chills, cough, dyspnea, palpitations, chest pain, nausea, weight gain, edema, or urinary complaints. She is, however, experiencing mild, general fatigue and a “scratchy throat”; otherwise there are no systemic symptoms. She is worried that her “cancer has come back.”
A:
Other medical history
- Hypothyroidism and hypertension
- History of deep venous thrombosis (DVT) attributed to her cancer; was on warfarin but “held” last week for her port removal surgery.
- Remote history of cholecystectomy
- No known drug allergies
- No history of myocardial infarction, congestive heart failure, stroke, or diabetes
- No recent international travel
- Current medications: anastrozole, hydrochlorothiazide, levothyroxine, calcium, warfarin, epoetin alfa, and acetaminophen
Family and social history
- Family history is significant for coronary artery disease late in life in her parents
- No family history of cancer, blood dyscrasia, or immunocompromise
- Formerly a smoker, only recently quit
- Moderate caffeine intake (coffee)
- Employed as a banker
Physical examination
- Temperature 99.7°F, pulse 92, respirations 20, blood pressure 122/74 mm Hg, weight 130 lbs
- Alert, oriented, no distress, full affect
- PERRLA (pupils equal, round, reactive to light and accommodation), extraocular motions intact, cranial nerves II–XII intact, mucous membranes moist, pharynx clear, no carotid bruits, minimal cervical adenopathy
- There is a tender, ill-defined mass on the left side of the neck, extending from angle of the mandible to the clavicle behind which it disappears
- Heart regular without murmurs or enlargement
- Lungs clear to auscultation in all fields
- Operative site on the left anterior thorax (port removal) is clean, dry, nonerythematous, healing well
- Abdomen is soft, nontender, nondistended, no organomegaly, normal bowel sounds
- Extremities show no significant edema or venous distention
A:
Lab results
- White bloods cell count elevated at 13 (3.9–10.9), 76% neutrophils with no bands
- Mild anemia of 11.3 (11.7–16.0)
- International normalized ratio (INR)= 0.94
- Blood cultures are pending
- Rapid strep test is negative
Next step: Order imaging studies
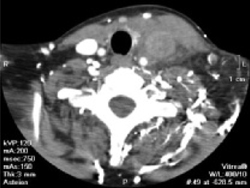
This particular presentation prompts you to order a computed tomography (CT) scan of her neck and chest, looking for a specific pathology (FIGURE 1).
When the scan is complete, the radiologist calls and confirms that there is occlusion of the left internal jugular vein, brachiocephalic vein, and a portion of the left subclavian vein with thrombosis.
A second CT of the chest again reveals the thrombosed veins, but there are no filling defects suggestive of pulmonary emboli or peripheral infiltrates or cavitary lesions suggestive of septic emboli (FIGURE 2).
The details. Thrombosis of the left internal jugular vein extends from the jugular siphon to the left subclavian vein. A portion of the left subclavian vein and probably the left brachiocephalic vein are also thrombosed. Numerous collaterals appear in the neck base. The left internal jugular vein measures 2.0 cm in diameter; the right measures 1.5 × 1.1 cm. There is also mild wall thickening of the internal jugular vein and infiltration of the surrounding fat—suggestive of septic thrombosis. No soft-tissue abscess is seen in the neck. The right internal jugular vein is normal. No definite thrombus is seen in the left jugular siphon or sigmoid sinus.
The parapharyngeal spaces are symmetric, though the infiltration of the fat around the left internal jugular vein is causing soft-tissue swelling and possibly mild tracheal deviation. The airway is not compromised. The superior mediastinum is grossly unremarkable. The upper lungs are clear.
A:
You vaguely recall that jugular thrombophlebitis is associated with some syndrome, so you turn to UpToDate and do a search on “jugular thrombophlebitis.”
There you learn that Lemierre’s syndrome, also known as necrobacillosis, is septic thrombophlebitis of the jugular vein. It most commonly develops following pharyngitis, and has been associated with dental microbes.1,2
Similar syndromes of suppurative thrombophlebitis may also occur in peripheral veins, associated with intravenous catheterization (especially PICC lines3), the superior and inferior vena cava, always associated with central lines,4 and the ovarian veins.5
FIGURE 1 Thrombosed veins