Medications
Among the 470 patients with a confirmed diagnosis of migraine who participated in Phase 2, the most common medications used to treat headaches during the 3 months prior to the study were over-the-counter medications (70% of patients) (TABLE 1). Fewer than one in five patients (19%) reported treating their pre-study headaches with migraine-specific triptan therapy.
At the beginning of Phase 2, primary care providers changed the headache medication regimen of 197 of these patients (42%). Of the 205 total changes to medication regimens, 72% involved adding a triptan; 10% involved adding other medications; 11% involved discontinuation of a medication; and 7% involved dose adjustment.
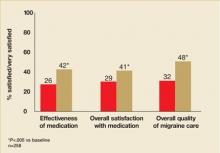
The changes to medication regimens were associated with significant improvement in satisfaction with medication in the subset of patients who finished Phase 2 and completed the end-of-study questionnaire (n=258). More patients indicated that they were satisfied or very satisfied with the effectiveness of headache medications used during the study than with headache medications used before the study (42% versus 26%; P<.005) (FIGURE 5). In addition, with respect to overall satisfaction with medication, more patients reported themselves to be satisfied or very satisfied with the medications used during the study than with those used before the study (41% vs 29%; P<.005) (FIGURE 5). Bothersomeness of side effects of migraine medication did not differ during the study versus before the study. Most patients (63%) reported themselves to be not at all bothered by medication side effects both during the study and before the study.
FIGURE 5
Percentage of patients who were satisfied/very satisfied with medication and migraine care
Quality of care
The proportion of patients indicating that they were satisfied or very satisfied with the overall quality of migraine care was significantly higher for care received during the study than care received before the study (48% vs 32%; P<.001) (FIGURE 5).
Impact of headache
Patients’ HIT-6 scores reflected significantly less impact of headache at the end of Phase 2 compared with the beginning of the study. The percentage of patients whose headaches impacted their lives substantially or very severely was 75.3% at enrollment compared with 68.8% at the end of the study (P<.05).
Patients with pre-study migraine diagnosis vs those without
Of the 470 patients in the Phase 2 sample, 230 reported a pre-study diagnosis of migraine and 240 report no pre-study diagnosis of migraine. Patients who reported a pre-study migraine diagnosis compared with those who did not appeared to have more severe migraine at baseline as reflected by a higher frequency of severe pain, a longer duration of typical migraine attacks, and higher frequency of HIT-6 scores reflecting substantial or very severe impact of headaches (TABLE 3).
Patients with no prior diagnosis were significantly less satisfied with care and medication at baseline than patients with a prior diagnosis. While satisfaction increased and headache impact decreased from baseline to the end of Phase 2 both in patients who reported a prior diagnosis and those who did not, improvement was greater in those without a prior diagnosis (TABLE 3).
Acknowledgments
Some of the data described in this manuscript were presented at the 47th Annual Meeting of the American Headache Society, Philadelphia, Pennsylvania, United States. The study described in this manuscript was funded by GlaxoSmithKline. The authors acknowledge Jane Saiers, PhD, for assistance with writing the manuscript. Dr. Saiers’ work on the manuscript was funded by GlaxoSmithKline.
CORRESPONDENCE
Stephen Landy, MD, Wesley Headache Clinic, 8974 Bridge Forest Drive, Memphis, TN 38138. E-mail: wesleyhead@aol.com