In general, there is greater justification for involuntary hospitalization with increasing “psychiatric dangerousness.” States vary on what requirements must be met for involuntary psychiatric hospitalization. Many jurisdictions have additional requirements to force psychiatric treatment; in some jurisdictions, forcing psychiatric treatment is not permitted.
Step 3: Determine the need for a surrogate decision-maker
The strength of the case for surrogate decision-making increases as decisional capacity decreases. A surrogate decision-maker is the person authorized to make decisions for a person who is not fully autonomous because of impaired decisional capacity. The ethical justification for obtaining a surrogate is to respect the patient’s prior ability to be informed and make a choice. Some patients share decision-making with other family or friends and this should be respected.
In our view, a surrogate should be obtained for a patient with impaired decisional capacity even when significant “psychiatric dangerousness” is present and involuntary hospitalization or treatment is pursued. The principle of equal respect for persons supports the view that since incompetent patients with medical problems are afforded a surrogate, so should incompetent patients with psychiatric problems.
Some might argue that the judge ordering the mandatory hospitalization or treatment is the surrogate. However, others who know the patient better and are more familiar with their values are more likely to provide authentic substituted judgment. At the same time, safety concerns for the patient (in the case of suicidal intent) or others (in the case of homicidal intent) require that surrogate decision-making be restricted. Surprisingly, no law or regulation in the US, to our knowledge, mandates appointing a surrogate for a patient who is involuntarily hospitalized or treated.
Managing treatment refusal in practice
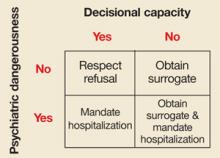
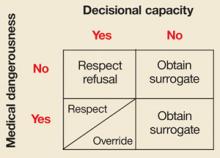
Evaluating decisional capacity and dangerousness leads to 3 possible decisions: 1) respect the treatment refusal, 2) obtain a surrogate, or 3) mandate hospitalization and possibly treatment. FIGURES 1 AND 2 depict such decisions for psychiatric and medical dangerousness, respectively. The important question during evaluation is not, “Is there decisional capacity or dangerousness?” but is rather, “How much decisional capacity or dangerousness is present?” Even if different evaluators agree which decision-making abilities are present or how much psychiatric dangerousness exists, a value judgment must be made to decide the threshold at which a surrogate is obtained or the court is petitioned for involuntary hospitalization or treatment.
Similarities in the assessments of medical and psychiatric dangerousness.
When a patient exhibits adequate decisional capacity and insufficient dangerousness of either type, treatment refusal is respected. When decisional capacity is judged to be impaired, a surrogate should be obtained regardless of the type of dangerousness that is present.
FIGURE 1
Decisional capacity and psychiatric dangerousness
In assessing a patient’s decisional capacity and level of psychiatric dangerousness, we depart from traditional practice (lower right-hand box) and recommend obtaining a surrogate decision-maker when the patient has inadequate decisional capacity.
FIGURE 2
Decisional capacity and medical dangerousness
In assessing a patient’s decisional capacity and level of medical dangerousness, our model considers the clinical context in judging whether to override or respect a patient’s decision (lower left-hand box).
Decisional capacity
Differences in the assessments. Two boxes in the figures deserve comment. First, the bottom right box of FIGURE 1 recommends a departure from current practice. As described earlier, we recommend obtaining a surrogate for patients who have impaired decisional capacity and are involuntarily hospitalized for psychiatric dangerousness. Second, in the bottom left box of FIGURE 2, treatment refusal by a patient who has decisional capacity and “medical dangerousness” may be respected or overridden depending on contextual factors. The long history of respect for liberty, and the requirement not to invade another’s body without consent generally supports respecting treatment refusal.
When decisions may be overridden in a patient with adequate decisional capacity and medical dangerousness. During a public health emergency, such as a tuberculosis or SARS outbreak, ensuring the public’s safety may outweigh respect for individual liberties. When someone with tuberculosis refuses treatment and has adequate decisional capacity, legal precedent and ethical justification exist to defend involuntary confinement or treatment in certain circumstances.6
When the threshold for adequate decisional capacity changes based on the level of medical dangerousness. With increasing medical dangerousness, a given level of decisional capacity may be regarded as inadequate, and treatment refusal may be appropriately questioned and consideration given to naming a surrogate.7,8 Alternatively, when there is little “medical dangerousness,” less decisional capacity may be required for a treatment refusal to be respected. This approach is controversial because it involves a modifiable notion of decisional capacity.9