- Consider progesterone to reduce the risk of recurrent preterm delivery (A).
- Consider calcium channel blockers (CCBs) as initial therapy for preterm labor; though these are Class C agents in pregnancy, CCBs are at least as effective as other agents and cause no known fetal or neonatal side effects (A).
- Consider tocolytic therapy for preterm labor, to prolong pregnancy for 2 to 7 days and thereby permit administration of antenatal corticosteroids and transfer to a tertiary center, if needed (A). Maintenance and recurrent use of tocolytics has not proven beneficial and should be avoided (A).
Despite diagnostic and therapeutic advances in premature labor, the rate of preterm delivery has increased in the United States. Preterm delivery, defined as birth before 37 weeks gestation, occurs in about 12% of pregnancies,1 and it is the leading cause of mortality among non-anomalous fetuses.2 Among premature newborns who survive, 10% to 15% have significant handicaps.3 Long-term sequelae include visual or hearing impairment, chronic lung disease, developmental delay, and cerebral palsy.4 The annual cost of premature birth in the United States exceeds $5 billion, and the rate of preterm delivery has increased in recent years.5,6 Specific maternal attributes increase risk of preterm delivery, though these factors need not be present for premature delivery to occur.
Standard techniques of physical diagnosis may not accurately detect preterm labor, either missing the diagnosis or prompting unnecessary hospitalization and treatment. Select imaging studies can more reliably indicate a true need for intervention.
This article reviews the risk factors for preterm birth, the tests available to accurately diagnose preterm labor, and the medications available to prevent or postpone premature delivery.
Risk factors
Preterm delivery is categorized as spontaneous or indicated. Almost 75% of preterm births occur after spontaneous preterm labor or preterm premature rupture of the membranes (PPROM). The remaining 25% of early births are elective due to conditions potentially harmful to either the mother or the fetus.7
Maternal risk factors for spontaneous preterm births are listed in Table 1.7-13 The risk factors for preterm labor and PPROM are similar, with the exception that those whose membranes rupture prematurely are more likely to be indigent, to smoke cigarettes, and to have bleeding in the current pregnancy.
Not all preterm births carry the same risks. Early preterm birth—delivery before 32 weeks— is associated with clinical or subclinical infection, short cervical length, and the presence of fetal fibronectin in the cervicovaginal secretions. It tends to recur and leads to long-term fetal morbidity. Late preterm birth—delivery after 32 weeks but before 37 weeks—is associated with increased uterine contractions, tends to mimic normal labor, and is less likely to cause peripartum morbidity.7 Despite these known risk factors, women can experience preterm labor without exhibiting any of them.
TABLE 1
Maternal risk factors for spontaneous preterm birth
| Risk factor | Odds ratio |
|---|---|
| Bacterial vaginosis at <16 weeks | 7 |
| Periodontal infection | 4 |
| Prior preterm birth | 4 |
| Prepregnancy BMI <20 | 3 |
| Interpregnancy interval <6 mo | 2 |
| Bleeding in 2nd trimester | 2 |
| African-American race | 2 |
| Psychiatric disorder | 1.6 |
| Cigarette smoking | 1.5 |
| Gestational diabetes | 1.2 |
| Sources: Iams 20027 ; Leitich et al 20038 ; Jeffcoat et al 20019 ; Moutquin 200310 ; Smith et al 200311 ; Kelly et al 200212 ; Hedderson et al 2003.13 | |
Increasing the accuracy of diagnosis
Uterine contractions before 37 weeks and concomitant change in cervical dilation or effacement as detected by digital examination comprise the standard definition of preterm labor.
Caveats with clinical evaluation
The problem with the definition above is that women may not perceive contractions, and that contractions are at times difficult to differentiate from benign Braxton-Hicks contractions of normal pregnancy. Moreover, digital assessment of the cervix lacks reproducibility when the dilation is <3 cm or effacement is < 80%.7 Clinical evaluation alone can easily suggest prematurity when it is absent and miss it when it is present.7
Imaging and lab evaluation more telling
The ability to diagnose preterm labor improves with the use of transvaginal cervical sonography or measurement of fetal fibronectin.
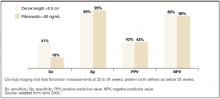
Lesser cervical length means greater risk. Likelihood of preterm delivery is inversely proportional to cervical length measured at 18 to 28 weeks. A length of ≤2.5 cm is the threshold for abnormal condition (level of evidence [LOE]: 2).6
Fibronectin detected late may mean delivery early. Fibronectin, an extracellular glycoprotein described as the glue that attaches the fetal membrane to the underlying uterine decidua, is normally absent in cervicovaginal secretions between weeks 22 and 37 of pregnancy. Its presence (50 ng/mL) between 22 to 24 weeks is a predictor of spontaneous preterm birth; its absence makes premature delivery unlikely (LOE: 2).
Imaging and test results justify management decisions. The predictive accuracies of abnormal cervical length and of the presence of fibronectin are depicted in the Figure .7 The major benefit of these two tests is when they are normal (cervical length >2.5 cm or negative fetal fibronectin), unnecessary intervention is avoided.14 If, for example, a patient is having contractions and the cervical length is greater than 2.5 cm, or fetal fibronectin is absent, tocolytics can be discontinued and hospitalization avoided.
FIGURE
Value of transvaginal cervical imaging and fetal fibronectin measurement in predicting spontaneous preterm birth