An efficient diagnostic framework
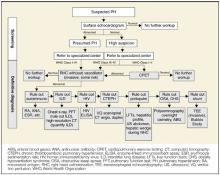
Proceed with a stepwise assessment ( Figure 1 ) of any patient exhibiting signs or symptoms suggestive of PH, particularly if there is an associated underlying condition or suggestive imaging study. Echocardiography (ECG) is usually the first test ordered, to detect thickening of the right ventricle or regurgitation of blood into the right atrium. ECG is neither sensitive nor specific for PAH. Not every patient will require the full work-up outlined in Figure 1 . The sequence and extent of testing depend on the clinical scenario. Cardiac catheterization is sometimes the last procedure, given its risks of invasiveness. A surface echocardiogram has a sensitivity of 79% to 100% and specificity of 60% to 98% for detecting PAH.15
FIGURE 1
Conceptual diagnostic framework for pulmonary hypertension
Functional assessment most important
Mean blood pressure above 25 mm Hg at rest or systolic pressure over 40 mm Hg in the pulmonary circulation constitutes pulmonary hypertension (see Pulmonary hypertension criteria ). However, the correlation of mean pulmonary arterial pressure to disease severity is not straightforward.16 Higher pulmonary artery pressure may portend better survival. The severity of pulmonary arterial hypertension is better determined by functional assessment. The New York Heart Association (NYHA) classification of dyspnea has been modified by the World Health Organization (WHO) to categorize PH by the severity of symptoms, which, unlike pulmonary arterial pressure, correlates well with survival. Even with epoprostenol treatment, functional class III patients have a survival of 60% at 7 years compared with less than 20% for class IV.17
Class I: Patients with pulmonary hypertension but without limitation of physical activity. Ordinary physical activity does not cause undue dyspnea or fatigue, chest pain, or near syncope.
Class II: Patients with pulmonary hypertension resulting in slight limitation of physical activity. They are comfortable at rest. Ordinary physical activity causes undue dyspnea or fatigue, chest pain, or near syncope.
Class III: Patients with pulmonary hypertension resulting in marked limitation of physical activity. They are comfortable at rest. Less than ordinary activity causes undue dyspnea or fatigue, chest pain, or near syncope.
Class IV: Patients with pulmonary hypertension with inability to carry out any physical activity without symptoms. These patients manifest signs of right heart failure. Dyspnea or fatigue may be present even at rest. Discomfort increases with any physical activity.
Pulmonary hypertension (PH) refers to elevated blood pressure within the pulmonary circulation. The term pulmonary arterial hypertension (PAH) encompasses a spectrum of disorders that cause PH with a common histopathology and pathobiology.56 The hallmark histopathologic lesion is plexogenic pulmonary arteriopathy.57
Normal mean pulmonary artery (PA) pressure is 12 to 16 mm Hg. PH is defined as a mean PA pressure greater than 25 mm Hg at rest, or greater than 30 mm Hg on exertion. Alternatively, systolic PA pressure greater than 40 mm Hg is also considered to be PH.58 Pulmonary arterial hypertension (PAH) is defined as a mean PA pressure greater than 25 mm Hg at rest (or 30 mm Hg with exercise), with a concomitant pulmonary capillary wedge pressure less than 15 mm Hg and a pulmonary vascular resistance (PVR) greater than 3 Woods units14 or 240 dyn•sec•cm-5.
Choosing from among improved therapeutic options
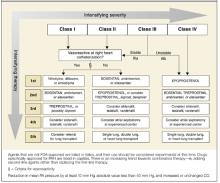
Main therapeutic goals are to prevent or reverse vasoconstriction, inhibit smooth muscle proliferation, impede thrombosis, and thereby reduce right ventricular failure. Newer pharmacologic agents have improved outcomes for patients and may even obviate the need for surgery. Treating the underlying cause of PH may be helpful, such as immunosuppression for SLE18 or positive pressure in sleep-disordered breathing.19 Table 2 outlines therapeutic options, and Figure 2 presents a strategy for applying these options.
FIGURE 2
Treatment algorithm for pulmonary arterial hypertension
TABLE 2
Treatment options for pulmonary arterial hypertension
| Medication | SOR* | Route | Adverse effects | Cost † | |
|---|---|---|---|---|---|
| Prostanoids | Epoprostenol | A | Intravenous | Line-related sepsis and thrombosis, jaw pain, fatal arrhythmia with sudden interruption | $$$$ |
| Treprostinil | B | Subcutaneous | Site pain (85%), jaw pain | $$$$ | |
| Iloprost | B | Inhaled | Short half-life with intermittent benefit | ||
| Endothelin antagonists | Bosentan | A | Oral | Hepatotoxicity, teratogenicity, fluid retention | $$$ |
| Sitaxsentan | B | ||||
| Ambrisentan | C | ||||
| PDE5 inhibitors | Sildenafil | B | Oral | Short half-life, retinopathy | $$ |
| Vardenafil | I | Short half-life | |||
| Tadalafil | I | ||||
| Surgical options | Lung transplant | C | Complicated procedure, lifelong immunosuppression | $$$$ | |
| Atrial septostomy | C | Invasive procedure, hypoxemia | $$ | ||
| Conventional therapy | Diuretics | C | Electrolyte imbalance, dehydration, etc | $ | |
| Digoxin | C | Higher mortality with high serum level | $ | ||
| Warfarin | C | Bleeding diathesis, dosing difficult in liver disease | $ | ||
| Calcium channel blockers | C | Harmful in vasodilator nonresponders | $ | ||
| Note: The level of evidence implied by the strength of recommendation must not be confused with level of efficacy. Medications not currently approved by the FDA for any indication are listed in italics. Only epoprostenol, bosentan, and trepros-tinil are approved specifically for pulmonary arterial hypertension. | |||||
| *SOR = strength of recommendation. A = Data derived from multiple randomized clinical trials or meta-analyses; B = Data derived from single randomized clinical trials or from multiple randomized clinical trials with heterogeneous results; C = Data derived from small randomized studies or consensus opinion of experts;59 I = indeterminate, no data available, theoretical basis only. See “Evidence-based medicine terms” on page 995. | |||||