However, at break points in the classification system, marked changes in risk occur with a 1-point differential in score. For example, for major noncardiac surgery, no difference in risk is reported between 6 and 12 points (4%) and no difference between 13 and 25 points (12%), but risk triples from 4% to 12% by adding 1 point from 12 to 13 points.
MedRules’ third algorithm, Lee’s Simple Cardiac Risk Score,5 fits on 2 screens. The maximum Lee score is 6 points. However, 1 point yields a risk of about 1%, whereas “class IV” is 3 or more points, for which the risk according to Lee et al5 is 9.1% in the derivation set and 11.0% in the validation set. For 3 or more points, MedRules’ calculator indicates “at high risk, >10% risk of major cardiac complications.” At 2 points, the risk is estimated at 7%, regardless of which factors are selected. With either 0 or 1 point, the Lee calculator returns a “<1% risk of major cardiac complications,” even if that risk is abdominal aortic aneurysm repair or a positive exercise stress test.
Obviously, with a 6-point scale and essentially 3 risk categories (in MedRules’ implementation, <1%, 7%, >10%), the Lee algorithm is extremely insensitive to small changes in risk.
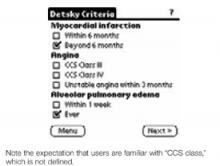
FIGURE 2
MedRules’ Detsky calculator
InfoRetriever
The 3 preoperative risk assessment tools on InfoRetriever (version 4.2 for Palm OS, 2002) comprise a tiny piece of this large (by palmtop standards) 2088K (2.1MB) collection of 90 clinical decision rules and other clinical tools. InfoRetriever’s opening screen offers a choice among “Clinical decision rules,” “Diagnostic tests,” and “History and physical.” After choosing “Clinical decision rules,” the user taps to invoke a drop-down menu, and then selects “CV–pre-op eval.” At this point, choices for 3 decision rules appear: “AAA surgery” (Steyerberg), “Non-vascular surgery” (Detsky), and “Vascular surgery” (L’Italien).
The major difference between InfoRetriever’s and MedRules’ Detsky calculators is that InfoRetriever divides surgery into major or minor procedures. The 2 algorithms also differ in asking whether unstable angina has been present in the past 3 months (MedRules) or past 6 months (InfoRetriever). Interestingly, Detsky’s 2 publications about his 1 study also differ in this regard.3,6 InfoRetriever defines angina class, eg, “class III: symptoms w/ level walking of 1 to 2 blocks or climbing ≥1 flight stairs,” whereas MedRules does not. Both of Detsky’s publications allow users to choose any desired pretest probability (overall operation-specific surgical risk) and, from a nomogram that includes the Detsky score, find the corresponding posttest probability (patient’s specific calculated risk).
Neither InfoRetriever’s nor MedRules’ Detsky calculators allow user input of pretest probability. InfoRetriever uses 2 stated, predetermined pretest probabilities (eg, 5% and 10%) and generates 2 corresponding, patient-specific posttest probabilities. MedRules uses a single, unstated pretest probability. Therefore, although both programs accurately calculate Detsky point totals, we conclude that neither completely reproduces the originally published material.
Comparing results between InfoRetriever’s and MedRules’ Detsky calculators, entering the same data for a patient whose MedRules’ Detsky result is 25/100 points, or a 20% risk of major cardiac complications, into InfoRetriever’s Detsky calculator results in “Moderate risk (II): Peri-operative risk of MI, CHF, or death is 15.9% given a pretest risk of 5%; 28.5% given a pretest risk of 10%.” Entering a higher-risk patient, MedRules’ Detsky calculates 40/100 points, and a “100% risk of major cardiac complications,” whereas InfoRetriever’s Detsky calculation produces “44% given a pretest risk of 5%, 62.3% given a pretest risk of 10%.” In contrast to MedRules, for this (and its other indices), InfoRetriever’s information screens discuss the patient population, provide a “quality score” (but no explanation of it) for the index’s referenced study, and specify the number of patients in the study. However, we believe this information is inadequate to guide clinicians in using the indices.
InfoRetriever’s vascular surgery risk index includes risk stratification based on whether a dipyridamole-thallium stress test was performed and, if so, whether a fixed defect, reversible defect, ≥1 mm ST segment depression, or any combination of these findings, was identified.8 The calculator requires the “complication rate at your institution (%),” without providing additional assistance. From the article by L’Italien et al,8 the reader can infer that the “average risk of a major perioperative cardiac event among vascular surgery candidates” would be acceptable as the input for the complication rate. However, the pretest probability for the specific type of vascular surgery (eg, carotid, infrainguinal) would be preferable (Table 2). Study end points were cardiac death, fatal and nonfatal MI, but not pulmonary edema caused by cardiac ischemia.