CASE 4
Trauma
A 33-year-old woman was brought to the ED after she was knocked off her motorbike by a car. A passerby found her unconscious and still wearing her helmet. En route to the hospital, the patient regained consciousness but had retrograde amnesia.
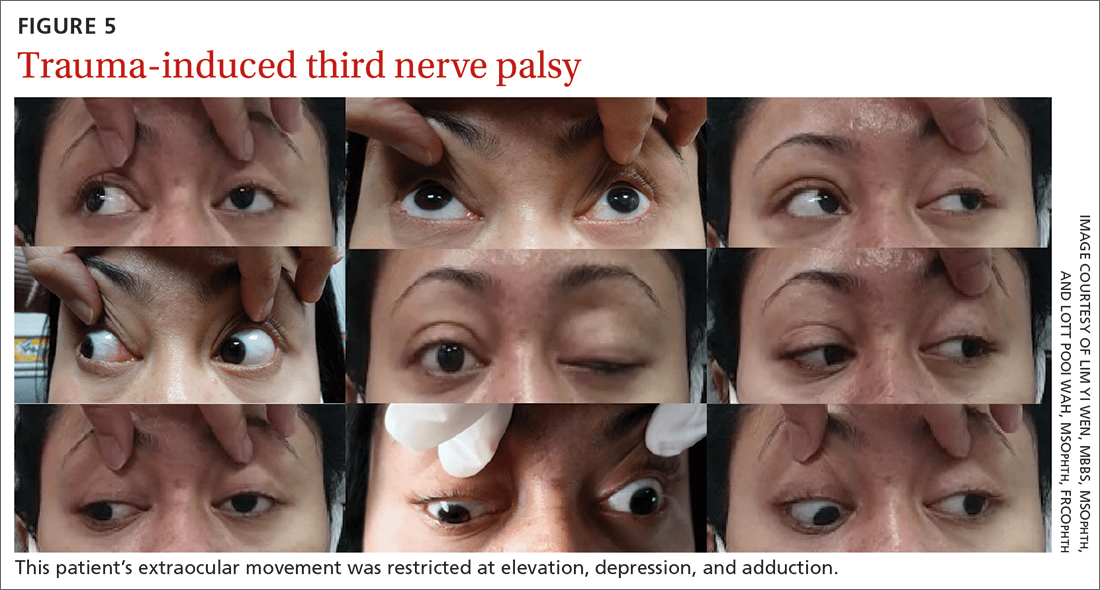
She was referred to us for evaluation of complete ptosis of her left eye. She was fully conscious during the examination. Her left eye vision was 6/9. Complete ptosis with exotropia was noted. Pupillary examination revealed a sluggish dilated left eye pupil of 7 mm with no reverse relative afferent pupillary defect. Extraocular movement was restricted at elevation, depression, and adduction with diplopia (FIGURE 5). All other CN functions were preserved.
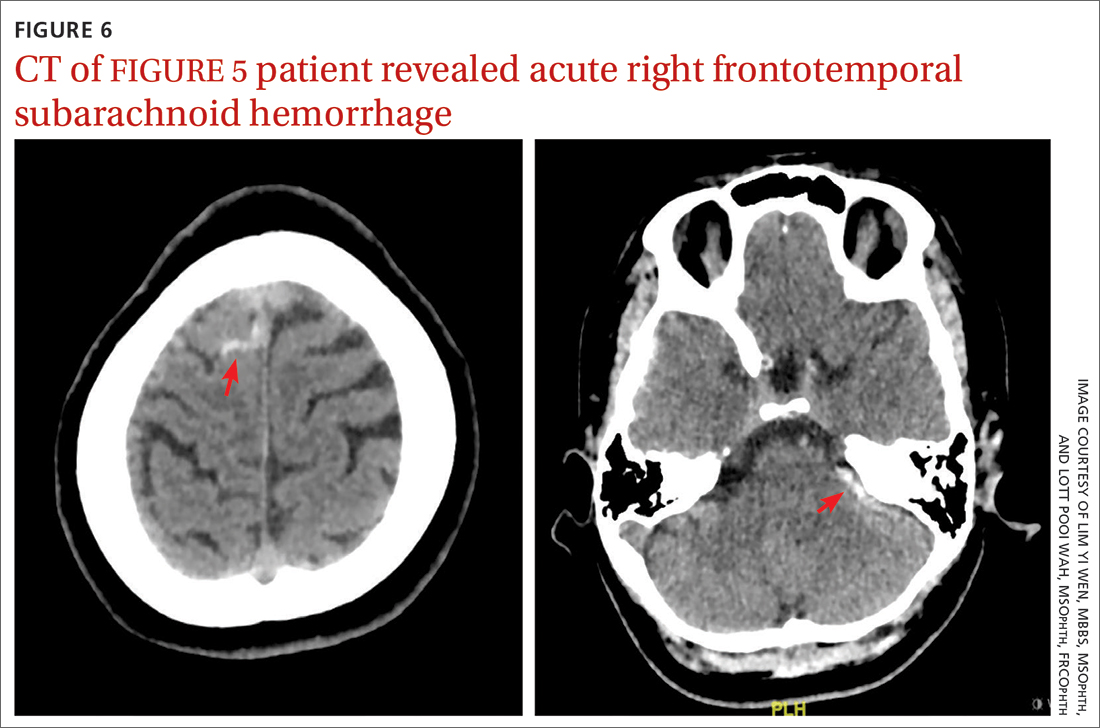
CT of the brain and orbit revealed acute right frontotemporal subarachnoid hemorrhage (FIGURE 6). There was no radiologic evidence of orbital wall fractures or extraocular muscle entrapment. She remained stable during the first 24 hours of monitoring and was given a diagnosis of left eye pupil-sparing complete TNP with traumatic mydriasis.
Repeat CT of the brain 5 days later revealed complete resolution of the subarachnoid hemorrhage. The patient's clinical condition improved 2 weeks later and included resolution of ptosis and recovery of ocular motility.
Key takeaways from the cases
Case 1: Herpes zoster ophthalmicus
Clinical diagnosis of HZO is straightforward, with painful vesicular lesions occurring along the trigeminal nerve (V1) dermatome, as was seen in this case. The oculomotor nerve is the CN most commonly involved; the trochlear nerve is the least-often affected.6 In a report from the Mayo Clinic, 3 of 86 patients with HZO had oculomotor nerve palsies (3.4%).7 A separate review from an eye hospital study stated that 9.8% (n = 133) of 1356 patients with HZO had extraocular muscle palsy, with TNP in 4 of the patients.8
Ocular complications such as blepharitis, keratoconjunctivits, or iritis occur in 20% to 70% of HZO cases.9 Ophthalmoplegia, which most often involves the oculomotor nerve, is seen in 7% to 31% of HZO cases (mostly in the elderly) and usually occurs within 1 to 3 weeks of the onset of rash.6 Our patient immediately underwent contrast CT of the brain to rule out meningitis and nerve compression.
Treatment with a systemic antiviral agent is crucial. Acyclovir, valaciclovir, and famciclovir are available treatment options, used for treating the skin lesions, reducing the viral load, and reducing the risk for ocular involvement or its progression. Our patient started a 2-week course of oral acyclovir 800 mg 5 times per day. Ophthalmoplegia is usually self-limiting and has a good prognosis. Time to resolution varies from 2 to 18 months. Diplopia, if present, resolves within 1 year.6 Our patient achieved full recovery of his extraocular movement after completing 4 weeks of antiviral treatment.
Continue to: Case 2