Calm mind, balanced mood
At the 8-week posttreatment assessment, which was the primary endpoint, the EA group had a mean reduction from baseline of 6.2 points (95% confidence interval, −6.9 to −5.6) in PSQI score.
There was a significant difference in PSQI score between the EA versus the SA group (−3.6 points; 95% CI, −4.4 to −2.8; P < .001) and vs the control group (−5.1 points; 95% CI, −6.0 to −4.2; P < .001).
The efficacy of EA in treating insomnia was sustained during the postintervention follow-up period when the EA group had a significantly greater reduction in PSQI score, compared with the SA group (−4.7; 95% CI, −5.4 to −3.9; P < .001) and the control group (−5.0; 95% CI, −5.8 to −4.1; P < .001).
Patients receiving EA also experienced significant (all P values < .001) improvement from baseline on secondary outcomes, including:
- Scores on the HDRS (−10.7; 95% CI, −11.8 to −9.7)
- Scores on the Insomnia Severity Index, (−7.6; 95% CI,−8.5 to −6.7)
- Scores on the Self-rated Anxiety Scale (−2.9; 95% CI, −4.1 to −1.7)
- Total sleep time, as recorded by sleep actigraphy (29.1 minutes; 95% CI, 21.5-36.7)
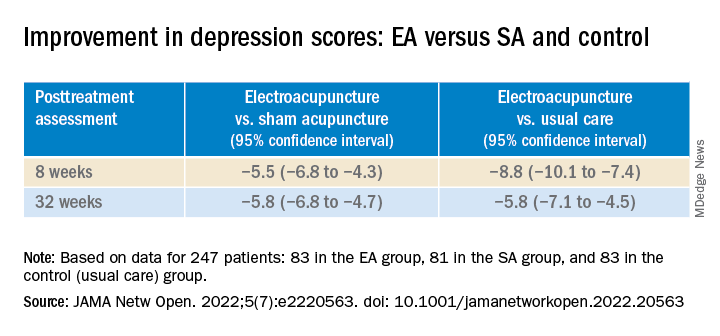
In addition, the EA group showed significant improvement in depression scores compared with the SA and control groups at both 8 and 32 weeks (all P values < .001).
Participants in the EA group also had a 4.2% (95% CI, 2.6% - 5.8%) higher sleep efficiency score at week 8, compared with those in the SA group (P < .001).
In addition, they had lower scores on the Insomnia Severity Index and the Self-rated Anxiety Scale, and longer total sleep time, compared with the control group at week 8.
None of the participants reported any serious adverse events.
“Our findings constitute subjective and objective evidence of the efficacy and safety of EA with standard care in treating comorbid depression and insomnia compared with SA with standard care or standard care alone,” the investigators wrote.
“The acupoints we used in this trial mainly act on calming mind, relieving negative mood, and balancing the yin-yang,” Dr. Xu added.
Viable adjunctive treatment
Commenting on the study, Albert Yeung, MD, ScD, associate director of the Mass General Depression and Clinical Research Program and associate professor of psychiatry, Harvard Medical School, Boston, said that, with the evidence from this study, “acupuncture and/or electroacupuncture could be a viable adjunctive treatment for depressed patients who suffer from insomnia.”
Dr. Yeung, who was not involved with the study, is the coauthor of an accompanying editorial.
“More well-designed studies are warranted to provide evidence for integrating holistic treatment in medicine,” he said.
The study was funded by grants from the National Natural Science Foundation of China, and Shanghai Municipal Health. The investigators and Dr. Yeung reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.