Although US is operator-dependent, it is the imaging modality of choice for identifying sialolithiasis10 because it can identify gland architecture, duct dilation, and both radiolucent and radiopaque stones. For patients in whom US findings are normal despite a convincing clinical presentation of sialolithiasis, CT should be performed because small stones can be missed on US.11
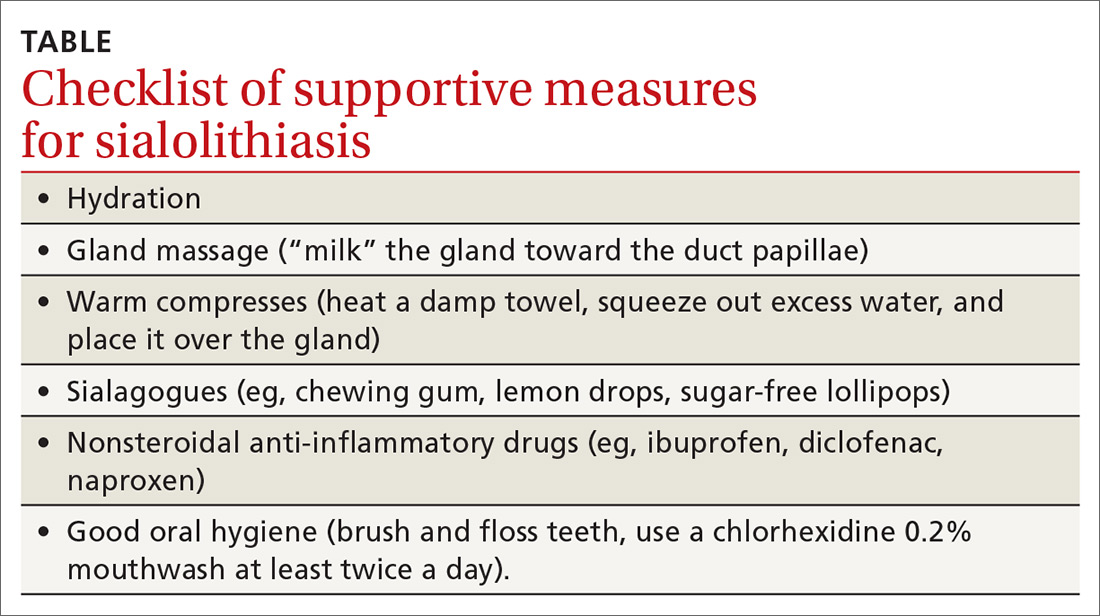
Supportive measures for sialolithiasis are listed in the TABLE. Reserve antibiotics for patients who have signs or symptoms of infection, including pyrexia, trismus, and malaise. A beta-lactam antibiotic, such as amoxicillin–clavulanate, 875 mg orally bid, or a cephalosporin, such as cephalexin, 500 mg orally qid, are appropriate first-line options. Clindamycin, 300 mg orally tid, or metronidazole, 500 mg orally tid, are acceptable alternatives. When signs or symptoms are persistent or recurrent, refer the patient for a surgical opinion.
Stones located in the floor of the mouth are usually excised through an intraoral approach. In the past, gland excision was advocated when a sialolith was found more proximally within the gland parenchyma. More recently, however, sialendoscopy, involving insertion of a small, semirigid endoscope into the salivary duct, has been shown safe and effective for removing a stone; successful removal, in as many as 80% of cases, increases to 90% when performed using a minimally invasive surgical technique.12 Although sialendoscopy is effective, the technique cannot always treat the underlying abnormality of the salivary gland; gland excision is therefore warranted in some cases.
Last, extracorporeal shock wave therapy is aimed at fragmenting salivary stones before retrieval. Results are variable, however, and treatment should be guided by an otolaryngologist.13,14
Sialadenitis (bacterial and viral infection). Acute suppurative sialadenitis occurs secondary to retrograde ductal bacterial infection. The parotid gland is most frequently involved,15 although submandibular sialadenitis is not uncommon. Patients usually present with sudden-onset unilateral, painful swelling.
Continue to: Pathophysiology involves...