The prevalence of a spectrum of bipolarity in the community has been shown to be 6.4%.1 Depressive episodes predominate in bipolar disorder (BPD),2 with patients spending less time in manic or hypomanic states.3 Not surprisingly, then, depressive episodes are the most common presentation of BPD.
The depressive symptoms of BPD and unipolar depression, or major depressive disorder (MDD), are similar, making it difficult to distinguish between the disorders.3 As a result, BPD is often misdiagnosed as MDD.4,5 Zimmerman et al point out that “bipolar disorder is prone to being overlooked because its diagnosis is more often based on retrospective report rather than presenting symptoms of mania or hypomania assessment.”6
Accurately recognizing BPD is essential in selecting effective treatment. It’s estimated that approximately one-third of patients given antidepressants for major depression show no treatment response,7 possibly due in part to undiagnosed BPD being more prevalent than previously thought.4,8 Failure to distinguish between depressive episodes of BPD and MDD before prescribing medication introduces the risk of ineffective or suboptimal treatment. Inappropriate treatment can worsen or destabilize the course of bipolar illness by, for instance, inducing rapid cycling or, less commonly, manic symptoms.
Screen for BPD when depressive symptoms are present
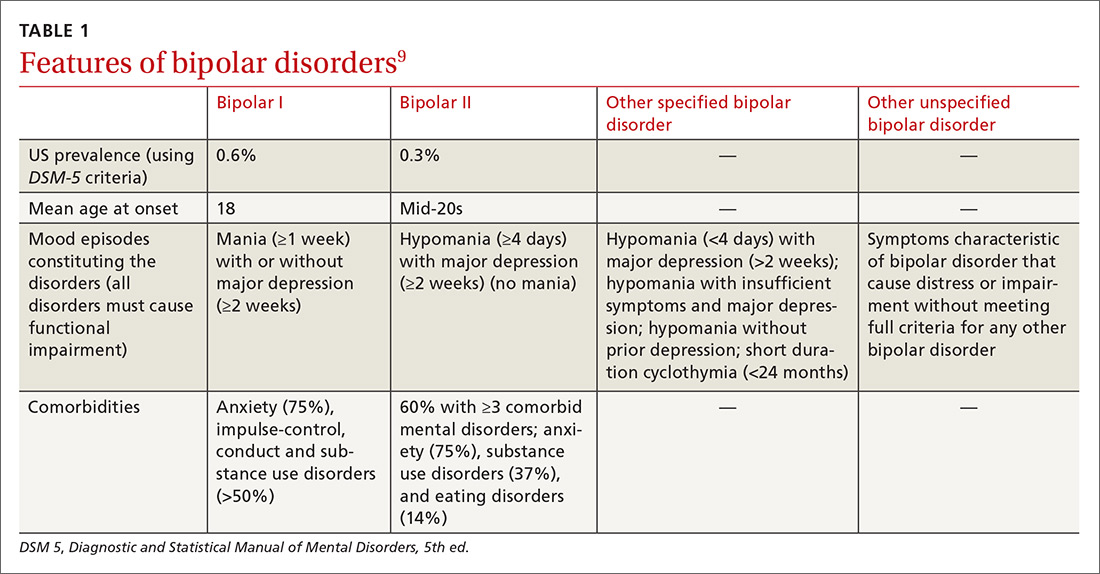
Identifying BPD in a patient with current or past depressive symptoms requires screening for manic, hypomanic, and mixed episodes (TABLE 19). Two brief, complementary screening tools — the Mood Disorder Questionnaire (MDQ) and the 9-item PHQ9—are helpful in this assessment. Both questionnaires (TABLE 28,10-14) can be conveniently completed by the patient in the waiting room or with staff assistance before the physician encounter.
The MDQ screen is for past/lifetime or current manic/hypomanic symptoms (https://www.integration.samhsa.gov/images/res/MDQ.pdf). A positive screen requires answering “Yes” to at least 7 of the 13 items on question 1, answering “yes” on question 2, and answering “moderate problems” or “serious problems” on question 3. One study done in the primary care setting found that the MDQ most accurately identified BPD when using a cutoff of 5 “Yes” answers to question 1.14 (During the clinical interview, discussed in a bit, confirming the positive MDQ items with DSM-5 criteria requires only current presentation or history of 3 symptoms of euphoric manic episode and 4 symptoms of irritable mania for bipolar I and II [may be less for bipolar spectrum].) Although the MDQ was originally developed to be clinician administered, later evidence and clinical experience found that it can also be self-administered.6,15
Continue to: The PHQ9 screens for...