TABLE 8
Case study 2: Self-monitored blood glucose (mg/dL) over the previous 2 weeks
| Day | Fasting | 2 h Post-breakfast | 2 h Post-lunch | 2 h Post-dinner |
|---|---|---|---|---|
| Tuesday | 135 | |||
| Wednesday | ||||
| Thursday | 196 | |||
| Friday | 152 | 174 | ||
| Saturday | ||||
| Sunday | 208 | |||
| Monday | 142 | 193 | ||
| Tuesday | ||||
| Wednesday | 130 | 156 | ||
| Thursday | ||||
| Friday | ||||
| Saturday | ||||
| Sunday | 151 | |||
| Monday |
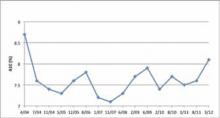
FIGURE 3
Case study 2: A1C levels for April 2004 to March 2012
Treatment Plan
- Discontinue metformin since LW’s serum creatinine is > 1.5 mg/dL.
- Initiate either basal insulin once daily in the evening or premix insulin at dinner.
- Ask LW to monitor his blood glucose and self-adjust insulin doses as appropriate.
- Stress the importance of exercise and proper nutrition; gain agreement on short-term goals for exercise and nutrition.
Barriers
LW’s physician recommends that his treatment plan be changed and insulin therapy initiated. LW quickly responds that previous changes to his treatment regimen have not resulted in his achieving an A1C < 7.0%. He also doubts that he can use a syringe to draw up the correct dose and then self-administer due to his arthritis. The following are possible responses his physician could use to address these concerns.
Patient concern: Repeated experience of failing to achieve glycemic control, ie, A1C < 7.0%
Physician responses:
- While achieving an A1C < 7.0% is a realistic goal that reduces the risks for vascular complications of diabetes, any reduction of A1C will be of benefit.
- I would like to work with you to implement a new plan that we both believe will enable you to improve your diabetes control and ideally achieve an A1C < 7.0%.
Patient concern: Self-administering due to arthritis
Physician responses:
- Instead of using a syringe and vial to draw up and administer insulin, I would like you to use an insulin pen device. As you can see, it is easy to handle and you can easily select the correct dose.
- If you choose to start on premix insulin, the pen device contains both types of insulin together in one dose.
Dosing
Treatment with basal insulin once daily in the evening can be initiated and titrated based on pre-breakfast blood glucose as in Case Study 1. Alternatively, treatment with premix insulin can be initiated at a dose of 12 U administered within 15 minutes of dinner initiation. The premix dose can be titrated using the algorithm employed in the 1-2-3 Study based on pre-breakfast blood glucose (TABLE 9).39 After 16 weeks, 41% of patients in the 1-2-3 Study achieved an A1C < 7.0% from a baseline A1C of 8.6%.
TABLE 9
1-2-3 Study algorithm39
| Pre-breakfast SMBG (mg/dL) | Adjustment of pre-dinner dose (U) |
|---|---|
| <80 | -3 |
| 80-110 | No change |
| 111-140 | +3 |
| 141-180 | +6 |
| > 180 | +9 |
| SMBG, self-monitored blood glucose. | |
Follow-Up Visit
LW began basal insulin 10 U in the evening. Over the next 5.5 months, he titrated his dose such that his current dose is 46 U (0.50 U/kg) in the evening. His current A1C is 7.3%. Review of his SMBG shows consistently high 2-hour post-lunch blood glucose levels. Although further increasing his basal insulin dose is an option, in most of the treat-to-target studies, the daily dose of basal insulin given once daily averaged between 0.4 and 0.6 U/kg.35,37,40,41 LW and his physician agree that adding rapid-acting insulin at lunch is the best option. The starting dose of rapid-acting bolus insulin is 4 to 6 U administered prior to the largest meal of the day or, as in this case, prior to the meal with the largest postprandial blood glucose excursion.42,43 Alternatively, the dose of rapid-acting insulin could be calculated as 10% of the total daily dose of basal insulin, which in this case is 5 U (10% x 46 U). The dose of basal insulin would be reduced by 5 U if the rapid-acting insulin is given at dinner in order to reduce the risk for nocturnal hypoglycemia. The dose of the bolus insulin can be titrated using the ExtraSTEP algorithm (TABLE 10).42 Alternatively, the SimpleSTEP algorithm can be used which does not require a 2-hour postprandial glucose measurement.42
TABLE 10
Algorithms for adjusting insulin aspart42
| ExtraSTEP algorithm | SimpleSTEP algorithm | |||
|---|---|---|---|---|
| 2-h Post-meal PG level (mg/dL) | Insulin aspart adjustment (U) | Pre-meal BG (mg/dL) | Bedtime BG (mg/dL) | Insulin aspart adjustment (U) |
| <72* | -2 | <72* | <72* | -2 |
| 72-144 | 0 | 72-108 | 72-144 | 0 |
| 145-180 | +2 | 109-162 | 145-180 | +2 |
| >180 | +4 | >162 | >180 | +4 |
| BG, blood glucose; PG, plasma glucose. *One or more PG values <72 mg/dL without obvious explanation. Reproduced with permission. Meneghini LF, et al. J Fam Pract. 2011;60(9 Suppl 1):S21-S28. Quadrant HealthCom Inc. Copyright 2011. | ||||
Plan
- Begin rapid-acting insulin 5 U at lunch.
- Continue basal insulin at 46 U in the evening.
- Ask LW to continue to titrate basal insulin based on the pre-breakfast blood glucose level and the lunch time bolus insulin dose based on the 2-hour post-lunch SMBG (ExtraSTEP); alternatively, adjust based on the pre-dinner blood glucose level (SimpleSTEP).
CASE STUDY 3
MB is a 46-year-old male who had not consulted a physician since having a physical examination 6 years ago. He presented 2 weeks ago with frequent urination (7-8 times/day) and feeling tired; he also noted losing 5 pounds (2.25 kg) over the preceding 3.5 months despite no changes in his diet. MB is a regional salesperson with an erratic schedule. During the week, he eats lunch and most dinners in a restaurant. On the weekend, he goes to a local bar with his friends. He does light yard work, but does not exercise regularly. He is a current smoker with a 36 pack-year history. Urinalysis shows ketonuria and microalbuminuria. His A1C reported back today is 10.8%, confirming a diagnosis of uncontrolled and symptomatic DM.