EVIDENCE-BASED ANSWER:
For adults with chronic rhinosinusitis (CRS), intranasal steroid (INS) therapy is more likely than placebo to improve symptoms (50% vs 32%; strength of recommendation [SOR]: A, systematic reviews).
Nasal saline irrigation (SI) alleviates symptoms better than no therapy (SOR: A, systematic reviews), but it’s probably not as effective as INS treatment (SOR: B, randomized controlled trial [RCT] with wide confidence interval).
Long-term (12 weeks) macrolide therapy doesn’t alter patient-oriented quality-of-life measures (SOR: A, systematic reviews).
Endoscopic sinus surgery improves CRS symptoms—nasal obstruction, discharge, and facial pain—over baseline (SOR: A, systematic reviews). Surgery and medical therapy appear about equivalent in terms of symptom improvement and quality-of-life measures (SOR: B, systematic reviews of low-quality RCTs).
EVIDENCE SUMMARY
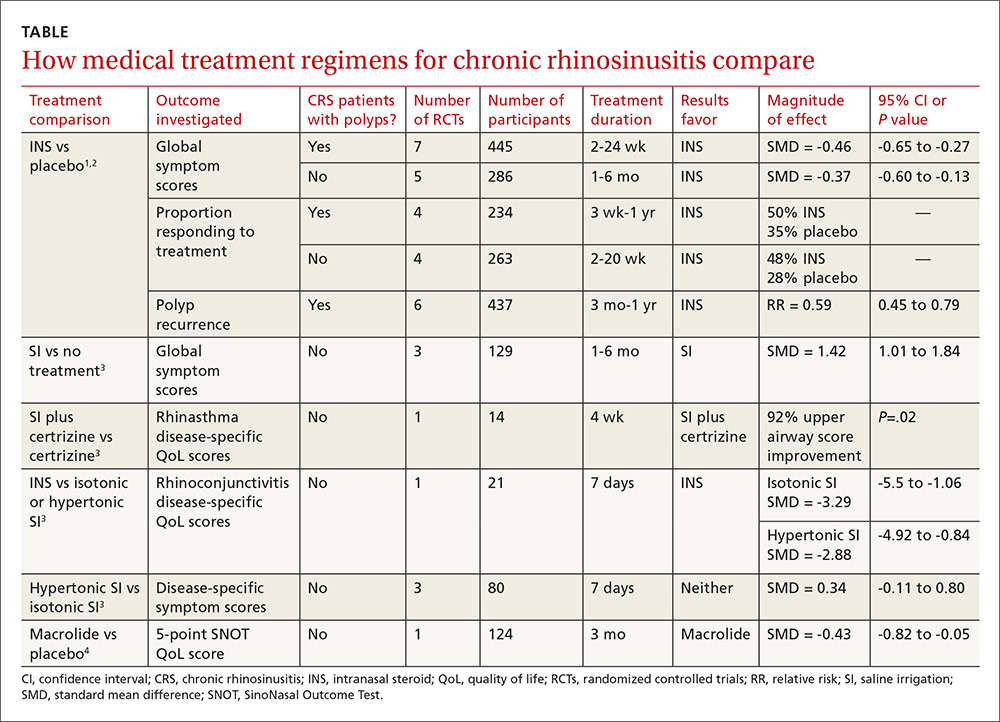
The TABLE1-4 shows the major results of the meta-analyses for the various medical therapy trials.
Two systematic reviews with meta-analyses evaluated treatment with INS for CRS with nasal polyps (40 RCTs; 3624 patients, mean age 48 years, 64% male) and without polyps (10 RCTs; 590 patients, mean age 39 years, 51% male).1,2 Trials reported sinonasal symptom outcomes differently and couldn’t be combined. In addition to reducing rate of polyp occurrence, for both CRS with and without polyps, key findings were:
- Global symptom scores were better for INS than placebo.
- Proportion of patients responding was greater for INS than with placebo.
There was no significant difference between adverse event rates with INS and placebo.
A systematic review and meta-analysis (8 RCTs, 389 patients) compared different SI regimens for CRS.3 The standardized mean difference was used to combine trials using various symptom outcomes. Key findings included the following:
- SI was better than no treatment.
- SI adjunctive therapy (with an antihistamine) improved disease-specific quality-of-life scores.
- SI was less effective than INS therapy for symptom improvement.
Hypertonic and isotonic saline yielded similar symptom scores. No adverse effects were reported.