Venomous bites and stings are responsible for significant mortality and morbidity worldwide.1 Interestingly, arthropods account for a higher percentage of deaths from envenomation than snakes, usually due to allergic reactions.2 In 2012, the American Association of Poison Control Centers (AAPCC) counted over 64,000 cases of bites and envenomations, some of which resulted in severe reactions.3 Fatalities from such exposures are typically rare, but severe systemic allergic reactions can occur. It is estimated that the incidence of anaphylaxis is approximately 50 to 2,000 episodes per 100,000 persons or a lifetime prevalence of 0.05% to 2.0%.4 Fortunately, most reactions are mild and only require supportive treatment. Envenomation and associated reactions, however, can present to the ED as life-threatening situations.5 Therefore, it is essential that the emergency physician (EP) be competent in the evaluation and treatment of a wide array of bites and stings.
Hymenoptera
The order Hymenoptera of the phylum Arthropoda can be divided into three subgroups that are medically relevant: (1) Apidae (Apids), which include the honeybee and bumblebee; (2) Vespidae, (Vespids) which include yellow jackets, hornets and wasps; and (3) Formicidae (ants).6
Bees and Wasps
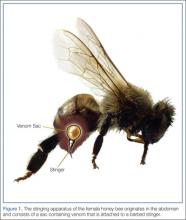
The main allergens in Apid venom are phospholipase A2, hyaluronidase, and melittin. Melittin, the main component, is a membrane active polypeptide that causes degranulation of basophils and mast cells. The allergens in Vespid venom are phospholipase, hyaluronidase, and antigen 5. As all Hymenoptera share some of these components, cross-sensitization may occur and individuals may be allergic to more than one species.7
The typical reaction to an insect sting is localized pain, swelling, and erythema; these symptoms generally subside after several hours. Little treatment is required other than analgesics and cold compresses. More extensive local reactions are also common, with swelling extending from the sting site over a large area.8 Symptoms typically peak within 48 hours and last as long as 7 days. The usual recommended treatment is nonsteroidal anti-inflammatory drugs (NSAIDs) (400-800 mg every 6-8 hours) and/or antihistamines (eg, diphenhydramine 50 mg orally every 6 hours as needed). Systemic steroids such as prednisone (40 mg orally daily for 2-3 days) are also beneficial and may be considered.2 Individuals exhibiting impressive localized reactions to stings tend to have similar responses after subsequent stings. The risk of anaphylaxis is approximately 5% per episode.9Occasionally after multiple stings, patients present with symptoms of a systemic toxic reaction. This is often seen in an Africanized bee attack. These so-called “killer bees” are hybrids of African bees that escaped from laboratories in Brazil in the 1950s and spread northward; they are found in most of the warmer US states. Their venom is not more toxic than that of any other bee, but Africanized honeybees are more aggressive and respond to a perceived threat in far greater numbers. The reaction that results from multiple stings is systemic and may resemble anaphylaxis. Common symptoms include nausea, vomiting, and diarrhea, as well as lightheadedness and syncope. Interestingly, urticaria and bronchospasm are not universally present, even though respiratory failure and cardiac arrest may occur. Other symptoms include renal failure with acute tubular necrosis, myoglobinuria or hemoglobinuria, hepatic failure, and disseminated intravascular coagulation (DIC).10,11 In addition, there have been reports of unusual reactions such as vasculitis, nephrosis, neuritis, encephalitis, and serum sickness. Late-appearing symptoms usually start several days to weeks after a sting and tend last for a prolonged period of time. Serum sickness tends to appear 5 to 14 days after exposure and consists of fever, malaise, headache, urticaria, lymphadenopathy, and polyarthritis.12 Of note, patients who have venom-induced serum sickness may be at risk for anaphylaxis after subsequent stings and may therefore be suitable candidates for venom immunotherapy.13
Anaphylaxis
The definition of anaphylaxis is not universally agreed upon. The American Academy of Allergy, Asthma and Immunology defines anaphylaxis as a serious allergic response that often involves swelling, hives, hypotension and, in severe cases, shock. A major difference between anaphylaxis and other allergic reactions is that anaphylaxis typically involves more than one body system.14 The clinical features of anaphylaxis from insect stings are the same as those from other causes, typically generalized urticaria, facial flushing, and angioedema. Abdominal cramping, nausea, vomiting, and diarrhea are also seen. Life-threatening symptoms include stridor, circulatory collapse with shock, and bronchospasm. Symptoms usually begin 10 to 20 minutes after a sting, and almost all will develop within 6 hours. Interestingly, symptoms may recur 8 to 12 hours after the initial reaction.15-18