Pulmonary Complications
Common Complications
Pleuritis. Many patients with SLE develop pleuritis, with or without effusion. This may be treated with nonsteroidal anti-inflammatory drugs, or corticosteroids if symptoms are more severe. Pleuritis is the most common respiratory complication of SLE, but due to the number of serious cardiopulmonary complications associated with SLE, pleuritis should be a diagnosis of exclusion.
Interstitial Lung Disease. Interstitial lung disease may be caused by SLE or may be medication-induced. This commonly presents as subacute or chronic dyspnea and/or cough. Patient workup may be done on an outpatient basis with high resolution chest CT and pulmonary function testing.
Pulmonary Hypertension. Patients with SLE may develop pulmonary hypertension, either directly due to SLE or from chronic thromboembolic disease. In general, pulmonary hypertension is managed as an outpatient, but may require emergent inpatient treatment if the condition is rapidly progressive or associated with right heart failure.
Shrinking Lung Syndrome. This condition may cause subacute or chronic dyspnea and pleuritic chest pain. Shrinking lung syndrome is caused by diaphragmatic dysfunction rather than from a primary disease of the lungs, and it is characterized by a restrictive pattern on pulmonary function testing and an elevated hemidiaphragm. Shrinking lung syndrome typically responds well to immunosuppressive therapy.16
Emergent Conditions
Pulmonary Embolism. A pulmonary embolism should be strongly considered in any patient with SLE presenting with the appropri ate clinical picture. Patients with APS are at particularly high risk for thromboembolic disease. However, even SLE patients without this APS are known to be at an increased risk of developing thromboembolism compared to the general public.17 Pulmonary embolism in SLE patients should be diagnosed and treated in the usual manner.
Pneumonia. Immunosuppressed patients are susceptible to opportunistic pulmonary infections as well as typical community pathogens. Fungal or mycobacterial infections may be suspected with a more subacute onset of symptoms.
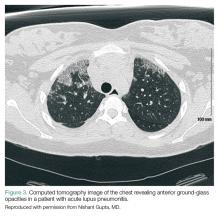
Acute Lupus Pneumonitis. This serious condition may present with severe pneumonia-like signs and symptoms, including fever, cough, dyspnea, hypoxia, and infiltrates on chest radiograph (Figure 3).
Acute lupus pneumonitis is caused by disease flare, and not by infection, although it may not be possible to distinguish it from pneumonia in the ED setting. The mortality rate of acute lupus pneumonitis is as high as 50%, and survivors often progress to chronic interstitial pneumonitis.1
Diffuse Alveolar Hemorrhage. A rare complication with a mortality rate of 50% to 90%, SLE patients who develop diffuse alveolar hemorrhage may present with fever, cough, dyspnea, and hypoxia.18 The condition may be suggested by infiltrates on chest radiograph, a drop in hemoglobin representing bleeding into the lungs, and/or hemoptysis. However, the absence of hemoptysis does not rule out diffuse alveolar hemorrhage, so clinical suspicion should remain high, even in the absence of this symptom.
Because emergent pulmonary conditions often present with similar symptoms, most patients with acute or new-onset symptoms will require admission for diagnostic workup (likely to include chest CT scan and/or bronchoscopy with bronchoalveolar lavage), as well as for close monitoring and initiation of treatment. If hypoxia or respiratory distress is severe, or if diffuse alveolar hemorrhage is suspected, admission to the intensive care unit (ICU) should be considered. We suggest that antibiotics be started in the ED when pneumonia is part of the differential diagnosis. As in the general population, coverage should be chosen based on the patient’s risk factors for antibiotic-resistant organisms. Initiation of corticosteroid therapy or other changes in immune therapy can be delayed until the EP consults with rheumatology and/or pulmonology services.
Cardiac Complications
Common Complications
Pericarditis. Pericarditis with or without pericardial effusion is very common in SLE patients and is usually related to lupus itself, rather than an infectious etiology. Patients may present with substernal, positional chest pain, tachycardia, and diffuse ST-segment elevation on electrocardiogram. Most effusions are small, asymptomatic, and discovered incidentally. However, among patients with symptomatic pericardial effusions, tamponade can be present in 21%.19 Corticosteroid therapy is often required to treat SLE-associated pericarditis, but colchicine is being explored as a possible steroid-sparing agent in this patient population.20,21
Valvular Abnormalities. Approximately 60% of SLE patients have valvular abnormalities detectable by echocardiography. The most common abnormalities in one study were valvular thickening or regurgitation.22 Many of these abnormalities occurred in asymptomatic patients and never progressed to clinical disease in a 5-year follow-up. However, patients with any valvular abnormality were more likely to develop complications, including stroke, peripheral embolism, infective endocarditis, need for valve replacement, congestive heart failure, or death.22
Emergent Complications
Acute Coronary Syndrome. Even in relatively young patients, acute coronary syndrome (ACS) should be considered in SLE patients presenting with chest pain, as this patient population has a 10-fold higher risk of developing coronary artery disease (CAD) than the general population, and SLE patients with CAD often lack traditional risk factors, such as advanced age, family history, or metabolic syndrome.1