Case
A 60-year-old morbidly obese man presented to the ED with a painless mass on his left thigh (Figure 1), which he stated had formed over a several day period 2 months earlier.
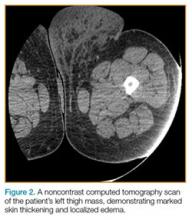
He further noted that although there had been no further growth in the mass since its initial formation, it had become debilitating and was interfering with his gait. The patient denied any drainage from the mass or any prior trauma to the area.On examination, the patient appeared well, with normal vital signs and a body mass index of 56 kg/m2. A computed tomography (CT) scan was obtained to further evaluate the mass (Figure 2), and dermatology services were consulted.
After examining the patient, the dermatologist diagnosed the patient with massive localized lymphedema (MLL). He was discharged home with a referral to an outpatient surgeon to discuss removal of the mass.Discussion
Massive localized lymphedema is a complication associated with morbid obesity. First described in 1998 by Farshid and Weiss,1 MLL is characterized by a benign pedunculated mass primarily of the lower extremity that slowly enlarges over years.2 The pathogenesis of MLL is currently unknown. Histologically, MLL contains lobules of mature fat with expanded connective tissue septa without the degree of cellular atypia in well-differentiated liposarcoma (WDL). Though similar to WDL, MLL can be differentiated by the clinical history of a slowly growing mass in a morbidly obese patient and examination findings of overlying reactive skin and soft-tissue changes associated with chronic lymphedema (eg, thickened peau d’orange skin).1,2
The diagnosis of MLL may be made clinically, and if there is no evidence of infection, the patient may be referred to a surgeon. If diagnostic uncertainty remains, biopsy and further CT imaging studies should be considered. The treatment for MLL is a direct excision if the mass is interfering with the patient’s gait. If left untreated, MLL can progress to angiosarcoma. Recurrence is possible, even after surgical excision.3