VACCINATION: DON'T FORGET ADULTS
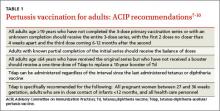
The 2 vaccines used to prevent pertussis are DTaP (diphtheria-tetanus-acellular pertussis) and Tdap (tetanus-diphtheria-acellular pertussis). The difference between the 2 is that the Tdap vaccine contains a reduced dose of the diphtheria and acellular pertussis vaccines. DTaP is designed primarily for children younger than 7 years of age. Tdap is given to older children and adults. The CDC and Advisory Committee on Immunization Practices recommend that children receive 5 doses of DTaP, one dose at each of the following ages: 2, 4, 6, and 15 to 18 months and at 4 to 6 years.7 All adults 19 years of age and older who have not yet received a dose of Tdap should receive a single dose regardless of when they last received any immunization for tetanus or diphtheria.7-10 A one-time Tdap booster should be given to all adults in place of a tetanus booster (TABLE 1).7-10
What about pregnant women? Tdap should be administered to every pregnant woman between 27 to 36 weeks gestation regardless of Tdap history.7,11 This strategy allows maternal antibodies to transfer to the infant, thus providing some protection to the newborn prior to pediatric vaccinations.
Is the vaccine becoming less effective? Since 1991, the number of cases of pertussis reported in previously vaccinated adolescents and adults has increased, which suggests waning immunity.12,13 Another recent trial investigating the acellular pertussis vaccine found that immunity decreases dramatically 5 years after the fifth dose.14
Recommendations on who should receive pertussis vaccination have been expanded to include adolescents and adults, including pregnant women and those ages 65 and older in close contact with infants, and this should decrease the overall incidence of disease through decreased communicability.15 Current recommendations call for a single adult vaccination; however, ongoing studies are evaluating whether a booster later in life might be necessary.15
DIAGNOSIS NEEDS TO BE CONFIRMED BY LAB TESTING
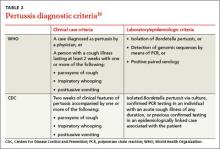
Any patient who reports having a persistent cough should be considered for pertussis testing and treatment, and any clinician who triages such patients should ask detailed questions about the characteristics and duration of the patient’s symptoms. However, while a prolonged cough is the hallmark of pertussis, there are many other potential causes of this symptom. Therefore, diagnosis of pertussis requires a combination of clinical and laboratory testing, because clinical parameters alone are neither sensitive nor specific enough for pertussis infection.
TABLE 216 outlines the clinical and laboratory diagnostic criteria for pertussis from the CDC and the World Health Organization. Suspect pertussis in a patient who’s had a cough for more than 14 days that includes an inspiratory “whoop.” In infants, pertussis should be suspected in those with symptoms that suggest cough and associated apnea.16 Order laboratory testing for any patients who have clinical signs or symptoms of pertussis.
Continue for the four methods of lab testing >>