Treatment. First rule out or treat any causes of acquired LQTS by taking a careful medication history and evaluating the patient’s electrolytes. Once these have been addressed, a beta-blocker is first-line therapy for symptomatic patients.5
Unfortunately, up to 20% of individuals treated with beta-blockers may continue to have syncope.5 For these patients, options include a left cardiac sympathetic denervation (LCSD) or placement of an automatic implantable cardioverter-defibrillator (AICD). An LCSD involves removal of the left-sided stellate and/or thoracic ganglia. This procedure can be used instead of, or in addition to, beta-blockers. If the patient’s syncope persists, AICDs are an option. AICDs can be lifesaving, but patients run the risk of adverse effects that include inappropriate shocks and infection.10 As the result of these therapies, mortality associated with LQTS has dropped to approximately 1%.11
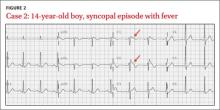
CASE 2 › A 14-year-old boy has a syncopal episode while at rest. A similar event occurred 3 years earlier; at that time, an echocardiogram and EKG were normal. For 2 days, he’s had a cough and low-grade fever. His temperature is 102ºF and he has a productive cough. Based on this EKG (FIGURE 2), what is the likely diagnosis? What is the significance of his fever?
The EKG abnormality and diagnosis. This patient’s EKG showed a type 1 Brugada pattern (FIGURE 2, ARROWS), which strongly supported the diagnosis of Brugada syndrome (BS). BS is an inherited condition caused by a genetic defect in cardiac ion channel function that leads to characteristic EKG changes and a predisposition to ventricular fibrillation.12 In this case, the fever likely unmasked these EKG findings.
The patient was transferred to a local hospital for treatment of community-acquired pneumonia, and ultimately received an AICD.
Etiology and epidemiology. BS was first described in 199213 and is a major cause of SCD, responsible for up to 4% of all cases of SCD, and 20% of cases of patients without structural heart disease.14 BS is more common in men, and the mean age of diagnosis is 40 to 45.15-18
Mutations in at least 17 cardiac ion channel genes have been linked to BS.19 The SCN5A gene—a cardiac sodium channel—is the most commonly implicated, but accounts for only 11% to 24% of all BS cases.15
Clinical features. Patients with BS may present with syncope, nocturnal agonal respirations, or ventricular arrhythmias.12 EKG findings include partial or complete right bundle branch block (RBBB) and ST segment elevation in right precordial leads V1 to V3.12 There are 2 Brugada EKG patterns, a type 1 cloved pattern as seen in our patient’s EKG and a type 2 saddleback pattern.20 EKG findings are dynamic over time and may alternate between normal, type 1, and type 2.20 Factors that modulate EKG appearance include fever, intoxication, vagal tone, electrolyte imbalance, and sodium channel blockade.12,20
Diagnosis requires a type 1 Brugada pattern on EKG plus a family history of BS, documented ventricular arrhythmia, or arrhythmia-related symptoms such as syncope.12 Patients with a type 2 Brugada pattern may undergo electrophysiology (EP) testing with Class I antiarrhythmic drugs to induce a diagnostic type 1 Brugada pattern.12,21 Patients who have Brugada EKG findings but none of the other diagnostic criteria are considered to have a Brugada pattern (rather than Brugada syndrome).12
The most concerning outcome of BS is ventricular fibrillation. The estimated annual rate of cardiac events is 7.7% among patients who have experienced an aborted SCD, 1.9% among those who have experienced syncope, and 0.5% in asymptomatic patients.18
Treatment. The only effective treatment for BS is placement of an AICD; however, complications of AICD placement cause significant morbidity.6 Ten years after AICD placement, 37% of patients experienced inappropriate shocks and 29% experienced lead failure.22 Recent modifications in device programming and the addition of remote monitoring have decreased complication rates.12,22
The decision to place an AICD is based on the patient’s prior symptoms, EKG findings, and other factors. Recent guidelines recommend an AICD for all patients with a type 1 Brugada pattern (spontaneous or induced) who also have had an aborted SCD, syncope, or documented ventricular arrhythmia.12
Management of asymptomatic patients with type 1 Brugada pattern remains controversial because the rate of cardiac events is low, although such events can be fatal. Asymptomatic patients with type 1 Brugada findings should undergo further EP testing, and should receive AICD only upon demonstration of inducible ventricular arrhythmia.12
TABLE 2
Arrhythmias associated with Wolff-Parkinson-White syndrome23
| Arrhythmia | EKG findings | Treatment—unstable patients | Treatment—stable patients (in preferred treatment order) |
| PSVT, orthodromic | Narrow QRS, loss of delta wave, rate 160-260 beats/min | Synchronized cardioversion | Vagal maneuvers, adenosine, calcium channel blockers, beta-blockers, digoxin, procainamide |
| PSVT, antidromic | Wide complex tachycardia | Synchronized cardioversion | Procainamide |
| Atrial fibrillation | Irregularly irregular (RR interval variable with no pattern), ventricular rates that can exceed 300 beats/min | Synchronized cardioversion | Synchronized cardioversion, procainamide |
| Atrial flutter | Flutter waves, rate normal to tachycardic depending on conduction rate | Synchronized cardioversion | Synchronized cardioversion, procainamide |
| Ventricular fibrillation | Rapid, erratic electrical impulses | Defibrillation | N/A |